Proximal Humerus Fractures
Shoulder surgery performed by an Adelaide-based orthopaedic specialist Dr Oscar Brumby-Rendell
Proximal humerus fractures affect approximately 5–6% of adult fractures, making them one of the most frequent upper-arm injuries, especially among older adults with osteoporosis.
These types of fractures are common in older adults, especially women with osteoporosis, and can also occur as a result of trauma, such as a fall or car accident. They are the fourth most common fracture in the elderly (>65 years old), with a 2:1 female-to-male ratio.
Fractures of the proximal humerus can make normal activities extremely difficult, as all movement at the shoulder is usually very painful.

Causes & Who’s at Risk of Proximal Humerus Fractures
Common causes of Proximal humerus fractures often relate to elderly accidents, high-speed trauma, or inherent causes like osteoporosis.
- These fractures commonly result from a fall onto an outstretched hand, particularly in elderly patients with low bone density.
- Younger patients may sustain these fractures through high-energy trauma like motor vehicle accidents or sports injuries.
- Osteoporosis significantly increases the risk (via bone fragility) especially in women over 60, who represent the majority of these injuries.
Patients with Proximal Humerus Fractures often present with:
- Severe shoulder pain, swelling, and bruising
- Limited mobility—notably difficulty lifting the arm
- In some cases, numbness or weakness, indicating possible axillary nerve involvement.
Diagnosis typically involves standard X-rays (e.g., AP, Y-view, axillary) to assess fracture patterns. A CT scan may be ordered for complex or multi-part fractures.
Fractures are often classified using the Neer system: ranging from 2-part to 4-part, based on displacement and fragment count.

Frequently Asked Question
Yes. A notable example is the Holstein–Lewis fracture, where a fracture in the distal third of the humeral shaft can lead to radial nerve entrapment. This may cause wrist and finger extension weakness and sensory loss.
Types of Proximal Humerus Fractures
There are 4 main types of proximal humerus fractures, based on the amount of fragments and if there was a dislocation.

Two part fracture
These fractures represent the ball of the shoulder breaking off in a simple pattern leaving only 2 parts to the injury. Depending on how displaced (distance between the parts) the fracture is helps decide the management and whether surgery is recommended.
Three or four part fracture
These fractures represent a multi-fragment fracture that also involves the rotator cuff muscle insertion points. There are attachment points at the front and side of the humeral head where the rotator cuff muscles attach, they are called the lesser and greater tuberosities. In 3- or 4-part fractures, 1 or both of these tuberosities also fracture, making the rotator cuff muscle deficient.
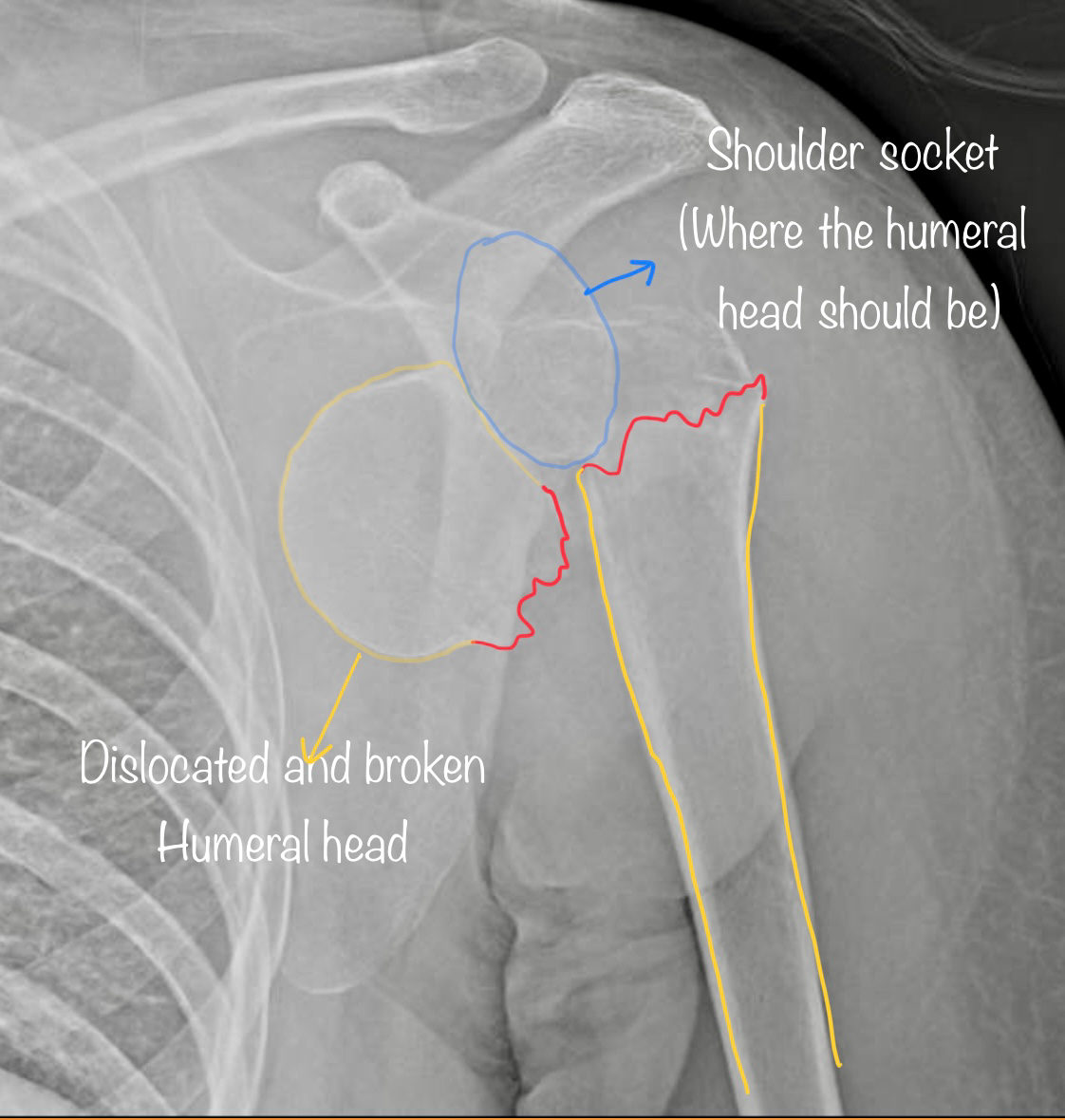
Fracture dislocation
This is a complex pattern whereby the humeral head has dislocated out of the socket but also suffered a fracture. This can also be in 2, 3 or 4 parts, and can be very complex. If the humeral head is stuck dislocated, this will always need surgery to put the shoulder back in the joint.
Treatment for Proximal Humerus Fractures
Non-surgical treatment
Proximal humerus fractures can be difficult to manage, as the shoulder is difficult to fully immobilise. Unlike the wrist, which can be put into a plaster or splint, the shoulder can only be supported in a sling which can still allow movement and be uncomfortable.
Typical non-surgical treatment will include:
- Sling immobilisation to support healing, typically for 4–8 weeks.
- Carefully managed early passive motion (e.g., pendulum exercises) to prevent stiffness and promote recovery.
- Regular follow-up X-rays to monitor alignment and ensure stability during healing.
Shoulder surgery
For more severe fractures or to allow an earlier range of motion, surgery may be beneficial. Fractures that often require surgery include:
- Fracture dislocations
- Locked dislocations
- Open or "compound" type fractures
- Fractures causing nerve damage - patients experiencing numbness or tingling
- Fractures where bone fragments are misaligned and cannot be corrected by a sling
Surgery on proximal humerus fractures can be complex, and most often, Dr Oscar Brumby-Rendell will organise a CT scan to use 3D planning. The 3D CT allows accurate visualisation of all the fragments and if the fracture is repairable. In some cases, particularly in more elderly proximal humerus fractures (>65yrs old), a joint replacement can be the best treatment option.
Dr Brumby-Rendell uses an incision at the front of the shoulder (anterior approach) and goes between 2 major muscles - the deltoid and pectoralis major. He will then use a specific plate system for the shoulder to reconstruct the fracture and put the fragments back in the right spot. This is called open reduction and internal fixation. If the damage is too severe, then he may need to conduct a joint replacement.
After the operation, the patients are treated with a shoulder sling and start a customised rehabilitation plan specific to their injury and surgery type. Most often, rehabilitation starts with gentle pendulum exercises and progresses to allow full active motion over the course of 6 weeks.


Why Choose Dr Oscar Brumby-Rendell
At the Adelaide Shoulder & Upper Limb Clinic, Dr Oscar Brumby-Rendell combines advanced orthopaedic expertise with a patient-centred approach to ensure optimal outcomes for proximal humerus fractures and other shoulder injuries.
-
Expert diagnosis and precise imaging – Dr Brumby-Rendell uses state-of-the-art imaging techniques, including X-rays, CT scans, and MRI where required, to accurately classify the fracture type and assess any associated soft tissue damage. This detailed assessment ensures that every treatment plan is based on a clear and complete understanding of the injury.
-
Tailored treatment plans – No two fractures are identical. Dr Brumby-Rendell develops personalised management strategies, whether non-surgical (such as immobilisation and guided physiotherapy) or surgical (including minimally invasive fixation techniques or complex reconstructions). Each plan takes into account fracture complexity, patient age, bone quality, lifestyle, and recovery goals.
-
Comprehensive rehabilitation support – Recovery from a shoulder fracture involves more than bone healing. Dr Brumby-Rendell provides ongoing guidance through every stage of rehabilitation, working closely with physiotherapists to promote safe, gradual progression from early mobility exercises to targeted strengthening. This holistic approach helps restore shoulder stability, flexibility, and long-term function, while minimising the risk of stiffness or re-injury.
By combining surgical precision, cutting-edge technology, and a deep commitment to patient care, Dr Brumby-Rendell ensures that each patient receives the highest standard of treatment from diagnosis through to full recovery.
Ready to learn more?
Watch more about Proximal Humeral Fractures with Dr Oscar Brumby-Rendell and other shoulder-related injuries.
Read more about them below:
Once you have a referral…
Book your consultation here.
