Shoulder Dislocation
Causes, Symptoms & Treatment Guide
Shoulder dislocation occurs when the head of the upper arm bone (humerus) pops out of the shoulder socket (glenoid). Despite its impressive mobility, the shoulder is prone to instability, especially after an initial dislocation.
This will cover everything you need to know about shoulder dislocation causes, symptoms, diagnosis, and treatment; including both non‑surgical and surgical options.

How the shoulder joint works
The shoulder joint (or glenohumeral joint) functions like a ball-and-socket system, allowing a long range of arm movement. Ligaments, tendons (including the rotator cuff), and the shoulder blade maintain joint stability.
So when the shoulder's muscular system is torn or damaged, the shoulder can lose its stability and dislocate from the socket. Damage to these structures can lead to weakness and dislocation.
Shoulder dislocation
When the humerus bone comes out of the socket, a dislocated shoulder occurs. There are two types of dislocations: partial (a subluxation) or full dislocations. An individual has a greater chance of experiencing a dislocation after their shoulder has dislocated once.
-
Subluxation (partial dislocation): The humerus slips partially out of the socket.
-
Complete dislocation: The humerus fully exits the socket.
-
Recurring instability often follows an initial dislocation.
Chronic shoulder instability
Shoulder instability is caused by the loosening of shoulder ligaments. This happens through injury or repetitive over-use.
Chronic shoulder instability describes the condition where the shoulder comes out of place frequently due to shoulder looseness. Individuals with this condition may experience shoulder dislocation during exercise or other forms of active movement.
Activities requiring repetitive overhead movements include volleyball, swimming, tennis and other sports. Such activities can stretch the ligaments in the shoulder, which can may decrease the shoulder's stability.
Causes of chronic shoulder dislocation and instability
Shoulder dislocation: Risk factors and diagnosis
Shoulder dislocations bring individuals discomfort, and often pain.
When the shoulder joint is corrected, the pain often improves considerably.
Some individuals can put their shoulder back into the joint themselves, but this practice is not recommended as it can cause nerve injury or further tearing. Ideally, medical professionals should reset a dislocation, as they can do this in a way that minimises the risk of further shoulder injury.

Dislocation or instability?
Shoulder dislocations result in visible deformity, meaning this condition is easy to diagnose.
Additionally, patients with a dislocation will not have the ability to move their shoulder. Rather, depending on the direction of dislocation, they will hold it across the body, to their side or above their head.
Signs of shoulder instability or dislocation include:
-
Intense pain and loss of motion during dislocation
-
Visible deformity in serious cases
-
Chronic symptoms between episodes: joint pain, clicking or “popping” sounds, and a feeling of looseness or slipping.
Risk factors for shoulder dislocation
Factors that increase your risk of shoulder dislocations include:
Age- Approximately half of shoulder dislocations occur in individuals between 15 and 29 years old.
Gender - Around 70% of dislocations happen in males.
Anatomy - The risk of shoulder dislocation is increased by loose ligaments, shallow joint sockets, and weak muscles in the shoulder.
Activity - Trauma from sporting injuries or falls causes many shoulder injuries.
Previous dislocation - Further dislocations are common as shoulder dislocations result in the tearing and stretching of muscles and ligaments which support shoulder structure.
Diagnosis of shoulder instability starts with a physical examination by your GP. They will ask about the history of your problem and your symptoms. The looseness or instability of your shoulder will be assessed via specific movement tests.
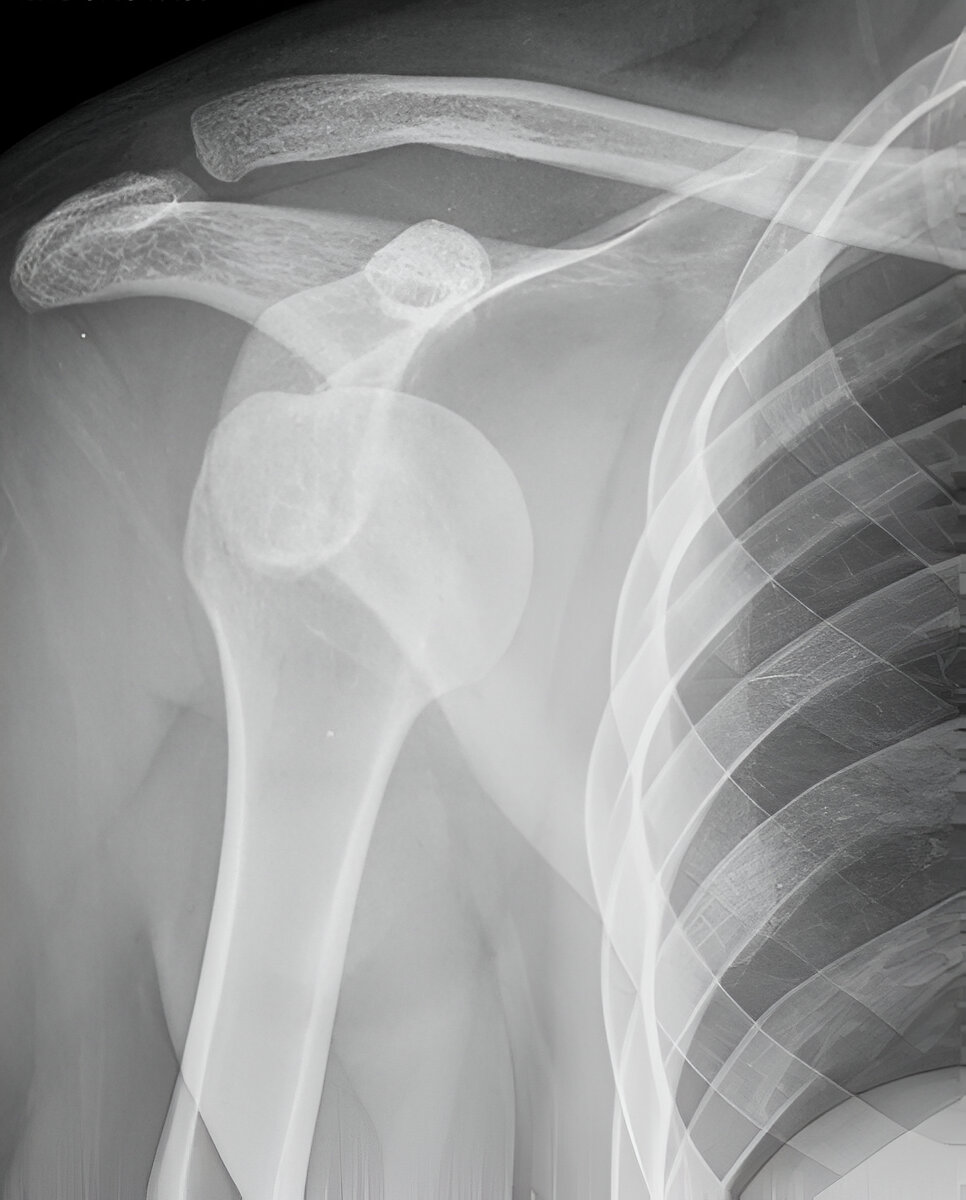
Diagnosis can be confirmed via imaging tests, which also identify any secondary issues. Such tests include X-rays (which observe the structure of your bones), and an MRI (which identifies ligament and tendon problems around the shoulder joint).
The joint may also be injected with dye, which is used to emphasise the studied structures in an MR arthrogram (MRA).
Book Your Shoulder Dislocation Appointment
Consult Dr. Oscar Brumby‑Rendell at Adelaide Shoulder & Upper Limb Clinic to explore tailored treatments for your chronic shoulder instability or dislocation problem.
Treatment options
Non-surgical treatments
Shoulder dislocation
There are two main steps in dislocation treatment: assessment and adjustment. Firstly, your GP will organise scans to assess the presence of fractures or risk of further damage. Before putting the shoulder in the correct position (reducing the shoulder), your doctor will evaluate bone, blood vessel and nerve damage.
CT or MRI/MRA imaging may be implemented in complicated dislocations to examine the surrounding muscles, soft tissues and cartilage for injury.
After the shoulder has been reduced, another X-ray is often carried out to verify that the shoulder has been placed in the correct position.
-
Immediate care after dislocation: Professional reduction (putting the shoulder back in place), followed by repeat imaging to ensure proper alignment
-
Conservative approach for chronic instability: Rest, rotator cuff strengthening, posture correction, and NSAIDs for pain and inflammation
Shoulder instability
Initially, chronic shoulder instability is treated with conservative measures, such as:
- Restricting shoulder movement and promoting rest to assist tendon recovery
- Strengthening rotator cuff muscles through shoulder exercises
- Moderating activity to reduce risks of further dislocations
- Consumption of painkillers and anti-inflammatory medication to decrease shoulder joint swelling and pain
If, after the above measures, the shoulder continues to dislocate or remains unstable, surgical intervention may be advised.
-
Ligament repair or tightening—to restore stability
-
Labrum reconstruction—for frequent dislocators
These minimally invasive procedures boast: -
95%+ patient satisfaction
-
Less than 1% complication rate
-
Faster recovery compared to open surgery
Surgical treatments
Surgery for shoulder dislocation
In cases where the shoulder is unstable and at high risk of re-dislocation, surgery may be suggested to reduce tissue and nerve damage and the risk of further dislocations.
Surgery generally entails tightening loose ligaments and repairing torn ligaments. To facilitate more efficient healing and reduce infection risks, orthopaedic surgeon Dr Oscar Brumby-Rendell executes this surgery arthroscopically (keyhole) where possible.
Arthroscopic surgery is carried out via numerous small cuts. A small camera and little medical instruments are introduced through these cuts, and Dr Brumby-Rendell guides the surgery using the camera's visual cues. This surgical method diminishes the need for a large wound.
The patient satisfaction rate of arthroscopic surgeries is 95%, with a complication rate of less than 1%.
Shoulder instability surgery
Shoulder instability and frequent shoulder dislocations can be corrected by repairing a torn labrum via surgery.
This surgery is also conducted arthroscopically (keyhole), with a tiny camera used to examine the inside of the shoulder and guide the operation. Small instruments designed for this surgery are implemented. High success rates, lower infection risks and faster healing periods are achieved through this surgical method.
Dr Brumby-Rendell conducts arthroscopic shoulder surgery, an outpatient procedure, at numerous locations surrounding Adelaide.
Frequently Asked Questions
Its wide range of motion makes the shoulder particularly vulnerable. Major causes include sudden impacts, falls, or repetitive overhead activity. Some individuals also have naturally loose connective tissues that further increase instability risks.

Shoulder surgery recovery
A shoulder sling will be used to immobilise your shoulder after surgery.
Generally, you will wear a sling for 2 to 6 weeks after your surgery (depending on your injury's severity and your specific surgery).
After this period, Dr Brumby-Rendell will advise a mild shoulder exercise plan to assist shoulder strength and movement post-surgery. These movements will be progressively introduced to your individualised rehabilitation plan.
For more information about shoulder surgery recovery, click here.
Ready to Learn More?
Want to learn more about shoulder conditions and treatments? Watch some of our videos below.
Once you have a referral…
Book your consultation here.
